Which Knee Replacement Implant Does Dr Mackie Use?
Between 2005 and ~ 2014 = Zimmer Nexgen Knee Replacement, using Patient Specific Instrument Techniques and then Computer Assisted Navigation (see below for information regarding navigation and robotic assisted surgery).
Between ~ 2014 and mid 2020 = Stryker Triathlon Knee Replacement, using Computer Assisted Navigation.
From mid 2020 = Zimmer Biomet Persona Knee Replacement, using Robotic Surgical Assistant (ROSA).
A recently "recalled" knee replacement (Exactech Knee) has not been used by Dr Mackie in public or private surgical practice.
Overview of Knee Replacements
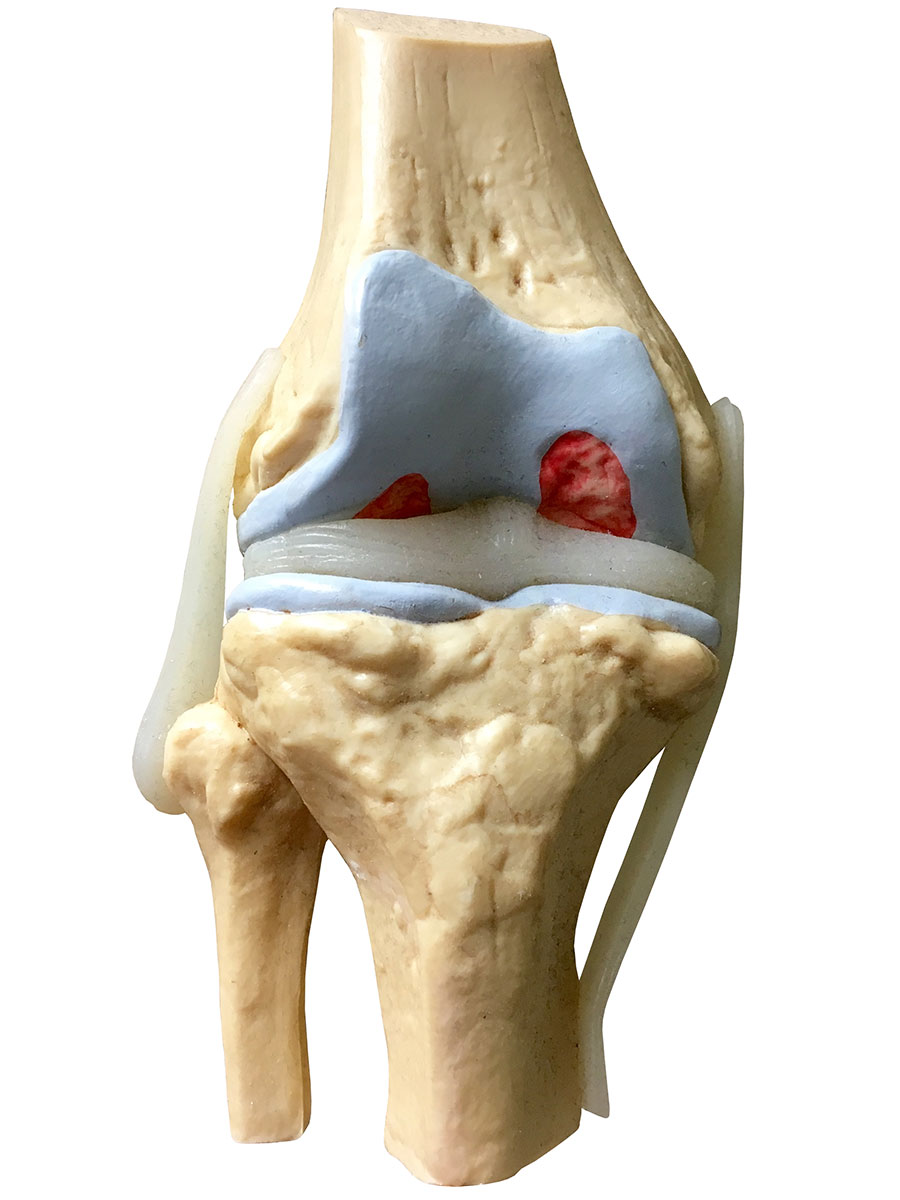
In a knee replacement, also known as knee arthroplasty, the worn (arthritic) surfaces of the bones of the knee are cut away and replaced by metal surfaces. A plastic liner is inserted between them, which functions as the new cartilage. A more detailed description of arthritis is within the "Conditions" section of the site.

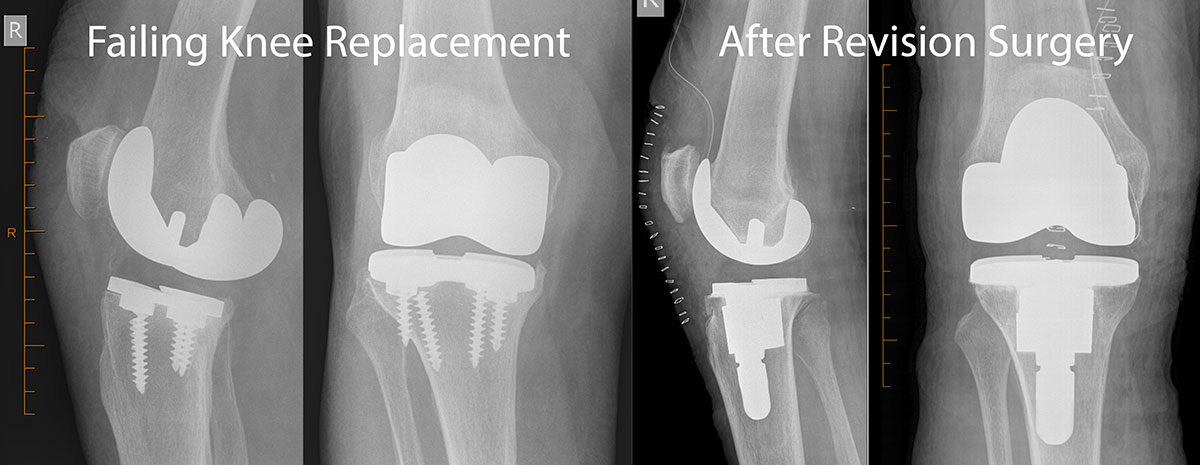
A knee replacement usually lasts many years, after which a revision operation can be done to replace it. However, revision operations are more difficult to perform than original knee replacements and the results are not always as successful. More than 90% of knee replacements are still functioning very well more than 10 years following surgery.
A partial knee replacement (unicompartmental) is sometimes used in patients in whom a discrete part of the knee is arthritic with the remainder of the joint in good condition. It is a slightly less invasive operation, with equally good outcomes and a slightly quicker return to activity. Only the diseased area is replaced. Fewer than 1 in 10 patients will have such a discrete area of arthritis which can be treated with a partial knee replacement.
Alternatives to Knee Replacements
Not everyone who has arthritis of the knee joint needs a knee replacement. Surgery is usually recommended only if non-surgical treatments do not help to reduce pain or improve mobility.
Knee replacement surgery is performed when a patient’s level of pain or functional disability warrants proceeding with surgery, acknowledging the risks of surgery, the potential costs, the recovery period and the potential for future surgery. It is important to have realistic expectations of the procedure and outcomes. Learn about the range of general treatment options for hip and knee arthritis.
How Long Do Knee Replacements Last?
Worldwide literature studies have shown that the majority of knee replacements will not require further surgery within the next 15 years. Some patients may unfortunately require reoperation within the first few months due to complications of the surgery. Within Australia a “National Joint Replacement Registry” has tracked the reoperation on knee replacements which have been inserted since 2000. Each year the registry is able to update surgeons on the statistical likelihood of patients requiring a reoperation to their knee replacement. Not surprisingly it shows that younger (and therefore more active) patients have a higher chance of reoperation on their knee replacement over the first 10+ years.
There are a number of reasons knee replacements are replaced or re-operated upon. The commonest (approximately 30% of reoperations) is gradual loosening of the metal prosthesis in the bone over the course of many years. Approximately 20% of re-operations are performed because of infection (which may be apparent within the first year, or may occur many years after knee replacement due to an infection spreading through the bloodstream). Twelve percent of re-operations are performed because of ongoing kneecap pain. The remaining re- operations are performed for a variety of reasons (including very rare implant-related faults or recalls).
Preparation for a Knee Replacement
If the planned surgery is more than 6 weeks away then patients may benefit from seeing a physiotherapist. The recovery period following surgery may be shorter in those patients who commence an exercise and activity program prior to surgery.
Patients may wish to arrange a modified living space at home (e.g. removing loose rugs or trip hazards, pre-preparing some frozen meals, ensuring they will be able to cope with their bathroom setup using crutches or a frame). Patients can discuss these matters with preadmission staff.
If any infections, cuts, or grazes occur prior to surgery in the leg being operated upon, or if patients suffer any other generalised medical illness, they should inform Dr. Mackie’s office. If urine tests performed at preadmission clinics demonstrate an infection or other tests are of concern it will be safer to delay elective surgery until the condition has been treated.
Prior to any surgery it is important to consider general health and risk issues. It is important to disclose any medical problems, medications taken and allergies to medications. Any blood thinning medications and medications for serious heart or lung conditions should be discussed prior with Dr. Mackie or the anaesthetist. It is necessary to cease aspirin / warfarin / plavix / iscover / pradaxa / fish oil or any other medications which cause excessive bleeding. Learn more about preparation for major surgery.
Anaesthetist
Patients will require a preoperative visit to an anaesthetist in order to ensure the anaesthetist is willing to proceed without further medical assessments. This visit will allow patients to discuss the type of anaesthetic that can be used for a knee replacement and postoperative pain management.
General Physician Review
If required, a referral to see a specialist physician will be arranged to deal with any medical conditions that may be improved pre-operatively (making the surgery and recovery safer). A general physician will be able to familiarize themselves with a patient’s medical conditions through a preoperative consultation and then be available in the immediate postoperative period to help prevent or treat any medical complications. Dr. Mackie will determine which patients may require this additional medical support.
Hospital Preadmission Visit
Before the operation, an appointment with a “preadmission service” at the hospital is usually arranged. At this appointment, patients will receive education about their time in hospital from Nursing staff. If required, a physiotherapist or occupational therapist will discuss home requirements. Aids and services can be planned before going into hospital. These might include handrails in the bath or shower, a raised toilet seat, and help with shopping or laundry.
This service also assists in arranging the following preoperative general health tests:
- ECG (Cardiograph) if needed
- Blood Tests
- Urine test to exclude infection
Day of Surgery
Typically, patients are required not to eat or drink for about six hours before a general anaesthetic.
For morning operations it is recommended that patients fast from midnight prior to surgery (no food or drink) although a small sip of water may be used to take normal medications. For afternoon operations it is recommended that patients have nothing after an early breakfast (~ 07:00 am). Some anaesthetists will permit clear fluids (water) to be consumed up until 2 hours prior to surgery.
Dr. Mackie will generally speak with patients prior to the anaesthetic on the day of surgery. He will use a texta-marker to confirm the side for operation and draw an arrow on it. In the period immediately prior to surgery patients will be asked multiple times by nursing and medical staff to confirm which knee is being operated upon, to avoid surgery to the incorrect side.
A Total Knee Replacement Operation
Total knee replacement is a major operation. It involves a stay in hospital of around four days, until it is safe to walk with the aid of sticks or crutches. The operation itself takes one to two hours, although most people are away from their room or ward for at least three hours.
The operation may be performed under a general anaesthetic (fully asleep), a spinal anaesthetic (using local anaesthetic injected into the lower back) or a nerve block (local anaesthetic injected around a nerve above the knee in conjunction with a general anaesthetic). During spinal anaesthesia the patient may remain awake but have no sensation from the waist downward.
Once the anaesthetic has taken effect, an incision, usually around 10-15cm long is made along the front of the knee. The diseased ends of the femur (thighbone) and tibia (shinbone) are precisely cut using carefully matched cutting guides. The cut bone surfaces are contoured exactly to allow a press-fit or tight insertion of the prostheses. Occasionally bone cement (like an acrylic glue) is used to help support the metal prostheses on bone. The femur and tibia invariably need to be replaced during surgery; although the back of the patella (kneecap) is assessed on an individual case bases and resurfaced with a plastic liner as required. The incision is closed (usually with dissolving stitches).

Modern Advances in Knee Replacement Surgery
Dr Mackie most often uses computer-assisted navigation of bone cuts during surgery. The operation may be performed via a slightly smaller wound than traditional knee replacements and with the same basic surgical techniques. Reflective trackers are affixed to bone and monitored by a camera linked to a computer. The computer is able to give immediate feedback regarding alignment of cutting guides. Additional trackers are used to accurately identify the centre of the hip, the centre of the knee and the centre of the ankle. Aligning all of these points when inserting a knee replacement helps to minimise the chance of instability or early wearing of the knee replacement. There are no additional investigations required prior to surgery and the costs of the disposable components of the computer-assisted system are met by the hospitals.
Recent analysis from the Australian National Joint Replacement Registry demonstrates that the performance of "computer assisted knee replacement" surgery has lowered the rate of revision surgery and this is thought to be due to the improved alignment obtained with the technique.
The implants have not changed much over many years (with some attempts to produce “better implants” backfiring on companies). Whenever a knee replacement is performed multiple sized implants are available to ensure the best fit for each patient by matching the size of the femur, tibia and the thickness of the intervening polyethylene.
What About Robotic Knee Replacement Surgery?
Dr Mackie is using a robotic surgical assistant arm. The term "Robotic Assisted Joint Replacement Surgery" has been recently popularised. It is important to differentiate the use of "Computer-Assisted Navigation" and robotic systems. A robotic arm uses computer programming and motors to help position a cutting saw or cutting guide on bone. The robotic arm still requires surgeon control / oversight and regular checks by the surgeon of the surgical plan. The robotic arm also relies on the same "Computer-Assisted Navigation" processes described above to permit the surgeon to make a surgical plan.
The most likley benefit to be gained from the use of a robotic surgical assistant arm is a more tailored soft tissue balancing of the knee, by using the combination of navigation and the workflows of the robotic arm. The soft tissues around the knee (ligaments, muscles, lining etc) require less surgical handling and many patients report reduced postoperative pain and a faster recovery after robotic arm assisted surgery. Despite this, there have been no large studies yet published which demonstrate significant longer term clinical superiorty of robotic-arm assisted surgery over the use of standard bone cutting blocks positioned via computer assisted navigation. Dr Mackie is using this modern technology to maximise patients' access to the aniticpated benefits.
The system used by Dr Mackie is the Robotic Surgical Assistant (ROSA) knee.
After a Knee Replacement
During the stay in hospital, every effort is made to keep discomfort to a minimum. The anaesthetist will explain the different kinds of pain relief that can be used. Most patients find that, after the first few days, they need only mild painkillers in tablet form.
In hospital, the physiotherapist will visit to help with exercises designed to promote recovery. Patients are generally encouraged to move their new knee from the first day after the operation. Some are asked to use a "continuous passive motion" machine, which continuously and gently moves the knee over an hour or two, gradually increasing the amount of movement each day. Dr. Mackie prefers patients to independently flex (bend) their knee to 90 degrees by time of discharge, as this permits comfortable sitting and the ability to rise from a chair. By the time they go home, patients are able to walk with sticks or crutches and will have learned how best to move about and manage daily tasks. However, they will need to make arrangements to be driven home.
Before discharge, a nurse usually gives advice about caring for surgical wounds, hygiene and bathing, and a follow-up appointment in the consulting rooms is arranged.
A period of time may be required in a rehabilitation ward prior to a final return home. This is determined by the preoperative health and mobility of patients and after assessment of how independent they may be in their home environment postoperatively. In-patient rehabilitation involves transfer to a different ward or hospital between 4 and 7 days post-operatively and a minimum of 1 week of additional in-patient time. Most patients however will be assessed as being safe to discharge directly home from ~ day 3 postop.
Once home, painkillers should be taken if needed, as advised. The knee will probably be sore for up to a few weeks. Most people find that they are able to move around their home and manage stairs, but some routine daily activities will be difficult for a few weeks. It's important to ask for help.
The exercises recommended by the physiotherapist are a crucial part of the recovery process, so it's essential to continue with them.
If patients are having any difficulties in achieving and maintaining greater than 90 degrees of knee bend and full knee straightening they must see a community based physiotherapist for assistance. When not walking or doing the recommended exercises, it's best to rest with the leg raised to help prevent swelling in the leg and ankle.
Patients who work will probably not be able to return for at least six weeks after the operation (2 weeks minimum if in office-based duties). They should not drive a car for 6 weeks (right knee replacement) and at least 2 weeks if a left knee replacement has been performed (automatic car only).
Dr. Mackie, the hospital or a GP should be contacted immediately if the operated area becomes red or develops a fluid discharge, or if the level of pain increases.
A follow-up appointment is made for 6 weeks post-surgery (with XRAY review). Most patients are able to walk moderate distances without crutches by this stage. The knee will continue to improve over a period of at least six months.
Side Effects and Complications of Knee Replacement Surgery
A planned knee replacement is generally a safe surgical procedure. For most people, the benefits in terms of pain relief are greater than the disadvantages. However, in order to give informed consent, anyone deciding whether or not to have this operation needs to be aware of the possible side effects and the risk of complications.
Side Effects
Side effects are the unwanted but usually temporary effects of an otherwise successful procedure. Examples of side effects include feeling sick as a result of the general anaesthetic and painkillers, and having a poor appetite to begin with.
In addition to these, some specific side effects can be expected:
- The new knee joint is likely to be uncomfortable on moving for many weeks.
- There is likely to be some temporary pain and swelling in the knee.
- It is quite common to have a swollen leg and ankle for up to 3 months afterwards.
- The operation will leave a 10-15cm scar over the front of the knee.
- Blood loss may require a transfusion of blood in a small number of patients.
- All patients will have a small patch of numbness to the outer side of bottom end of the wound.
- Many patients will notice an occasional painless “clunk” which is due to a subtle metal-on-plastic bump.
- In the longer term, the artificial joint will not last forever and, after years of use, a further operation may be needed.
Complications
Complications are unexpected problems that can occur during or after the operation. Most people are not affected, but the main possible complications of any surgery are excessive bleeding, infection or an unexpected reaction to the anaesthetic. Complications may require further treatment such as a further operation to stop bleeding, or antibiotics to treat an infection.
Complication rates are considerably higher in patients who:
- are smokers
- have diabetes
- use “disease modifying drugs” in rheumatoid arthritis
- have a Body Mass Index (BMI) greater than 35
Medical
Patients may suffer heart attacks, strokes, chest infections, urinary infections and other medical problems which usually reflect their general preoperative state-of-health. In rare circumstances patients may die as a result of medical conditions being exaccerbated by the stress associated with anaesthesia and surgery. Patients considered at-risk of significant medical issues will be referred prior to surgery to see a Medical Specialist Physician for assessment.
Infection
If patients experience increasing pain, swelling, redness, fevers or are generally unwell it is important to be reviewed early to ensure no infection has occurred. If infection is suspected most patients will be readmitted to hospital for antibiotics and may require a repeat operation to wash out the infection. Up to 1 in 100 patients may require repeated surgery (2 - 3 washout operations) for an infection, with many weeks back in hospital and up to 1 year on antibiotics. Very rarely amputations have been necessary to save a patient’s life because of severe infection.
Nerve Injury
All patients will have a patch of numbness just to the outer side of the bottom end of the wound. This is due to a small nerve running across the front of the knee having to be cut during knee replacement surgery and is usually not bothersome. The area of numbness reduces over many months. More significant nerve injuries are very rare.
Fractures
Occasionally, tiny cracks are made in the bone while fitting the new joint. These usually heal by themselves, but on rare occasions a fracture can result, needing additional treatment, such as prolonged bed-rest or a further operation.
Wound Healing
In up to 2% of cases the incision may not heal properly, increasing the risk of infection. Plastic surgery may be required.
Instability
In 1-2% of cases it is not possible to make the new knee fully stable and a knee brace may have to be worn. In less than1% of cases the kneecap becomes dislocated after knee replacement surgery.
Urine Retention
Following major surgery and anaesthesia the bowels may take a while to become active again and there may also be difficulty in passing urine. A urinary catheter may be inserted to enable urine flow. A urinary tract infection, requiring antibiotic treatment, may occur.
Stiffness
A build up of scar tissue occasionally restricts movement. A manipulation of the knee under anaesthetic (with several days in hospital) or rarely another operation may be performed to break down the scar tissue. Any patient who cannot maintain close to 90 degrees of movement beyond 4 weeks postop should inform Dr Mackie’s office. In rare cases, the loss of movement may be permanent.
Blood Clots
For up to six weeks after the operation, it is possible to develop a blood clot (known as a deep vein thrombosis, or DVT) in the veins of the leg. This clot can break off and cause a blockage in the lungs. In the majority of cases, this is treatable, but it can be a dangerous condition. Preventive drugs, or mechanical means to squeeze the feet should be used to reduce this risk whilst in hospital and a 100mg aspirin tablet daily for 6 weeks postop can reduce the risk.
Loosening
Artificial joints are subject to “wear & tear” of use and may loosen, crack or even break. Some joint replacements will require a revision operation by 10–15 years following surgery as per earlier information.