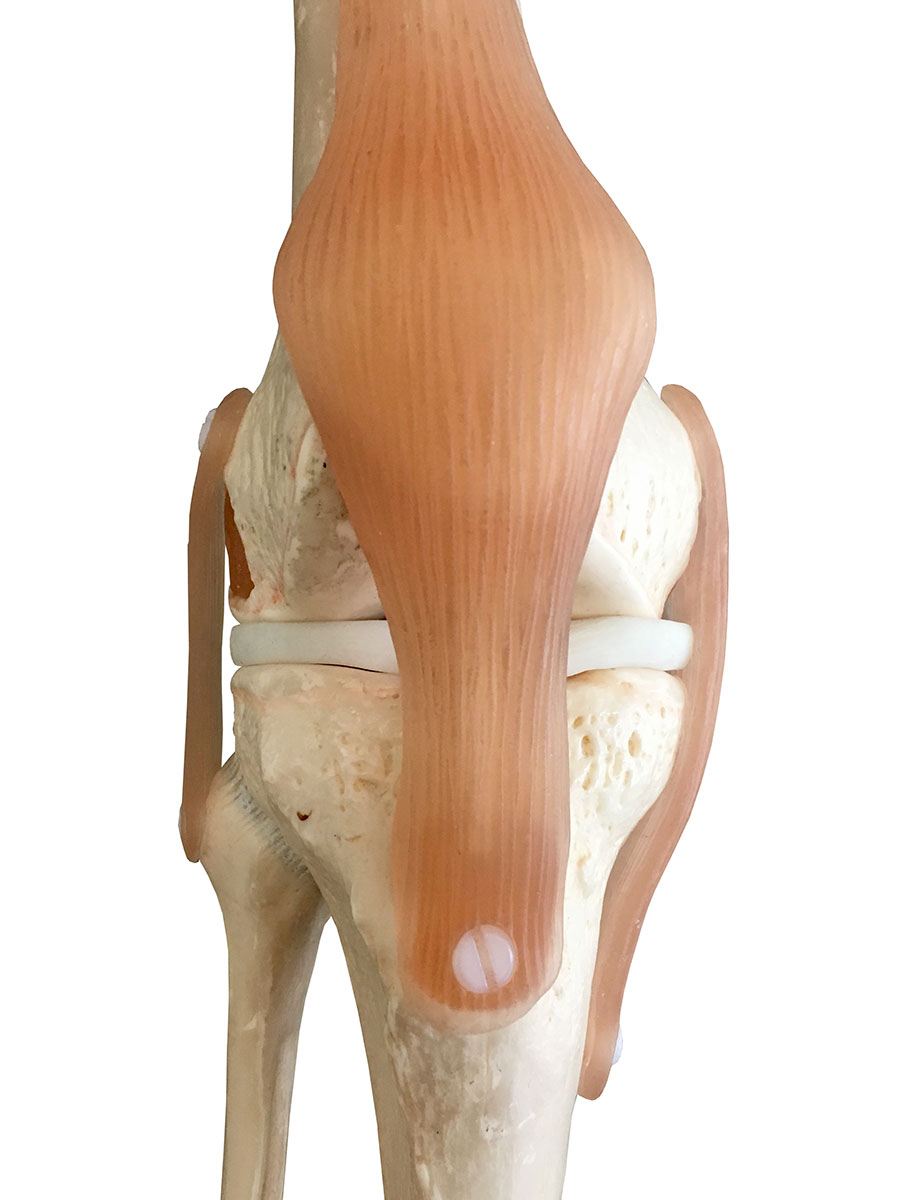
A Normal Knee Joint
The lower end of the femur (thigh bone) and upper end of tibia (shin bone) are covered by a firm articular cartilage surface (gristle) that is normally as smooth as a billiard ball.
A meniscus is a softer cartilage, which acts as a shock absorber. Meniscal structures are prone to tearing (especially after rotational stress on the knee or with overuse of the knee). Most knee arthroscopy operations are performed to deal with tears of a meniscus.
Ligaments stabilise the knee to allow normal range of motion.
Faults in any of these structures can be assessed by arthroscopy and may be treated.

About Knee Arthroscopy
Arthroscopy is a "key-hole" operation that is used to look inside and treat joints, especially the knee joint. It is performed through very small incisions in the skin, using a narrow telescope (arthroscope) attached to a video camera. Compared to open surgery, which involves a larger incision, keyhole surgery is less painful, carries less risk of infection, and enables people to recover more quickly.
An arthroscopy may be used to investigate knee problems, treat conditions such as arthritis and inflammation, take small samples of tissue, or repair damage to tissues and cartilage. The procedure is usually done as a day case - without the need for an overnight stay in hospital.
Not everyone who has knee problems will need to have an arthroscopy. In many cases, the problem can be diagnosed using non-surgical methods such as MRI (magnetic resonance imaging) and some problems can be treated via physiotherapy. Other conditions (especially more advanced arthritis) simply cannot be treated via arthroscopy.
Prior to Knee Arthroscopy
In general, prior to a knee arthroscopy little needs to be done preoperatively. Appropriate referrals are made at the time of surgical booking.
If patients wish to be involved in a physiotherapy program after the surgery it may be wise to see a therapist prior to surgery and to commence simple muscle and knee exercises.
If any infections, cuts, grazes occur prior to surgery in the leg being operated upon, or if patients suffer any other generalised medical illness, they should inform Dr. Mackie. It is safer to delay elective surgery until the condition has settled. Tests such as heart cardiographs and chest X-rays are only required for severely ill or elderly patients undergoing surgery
Typically, people are required not to eat or drink for about six hours before a general anaesthetic. For morning operations it is recommended that that patients fast from midnight prior to surgery (no food or drink) although a small sip of water may be used to take normal medications. For afternoon operations it is recommended to have nothing after an early breakfast (~ 07:00 am). It is necessary to cease aspirin / warfarin / plavix / iscover / pradaxa / fish oil or any other medications which cause excessive bleeding. Medications for serious heart or lung conditions should be discussed prior with Dr. Mackie or the anaesthetist.
Patients must bring any XRAYs or scans of their knee to the hospital with them, as the hospitals do not provide the computer access to scans that Dr. Mackie uses in his rooms. If XRAYs or scans are unavailable for viewing on the day of surgery, then the operation may be cancelled.
A Knee Arthroscopy
An arthroscopy is most often performed under a general anaesthetic as a day case. A spinal (regional) anaesthetic may be used after discussion with the anaesthetist. The operation can last from 30 minutes to over an hour, depending on how much work needs to done inside the joint. Having a general anaesthetic means that the person is asleep and feels no pain throughout the procedure.
Once the anaesthetic has taken effect, a small incision (around 5mm long) is made in the skin around the joint that is being treated. Sterile fluid is pumped inside to help produce a clearer picture of the inside of the joint. Another small incision is made for the arthroscope, which is about the thickness of a ballpoint pen.
Fluid is pumped into the knee to distend the space between the bones for better visibility. The knee joint is inspected in a systematic manner and those conditions that can be treated through the mini-incisions are addressed.
In many cases (in which treatment can be provided) small instruments are used to remove or repair damaged structures. Wherever possible a photographic record is made of the findings and a copy of the photographs provided to patients prior to discharge from hospital.
The fluid is drained out of the joint at the end of the procedure, although a small amount remains (accounting for swelling in the first few days). The incisions are closed with dissolving stitches and a compressive bandage applied to the knee
Meniscus Tears
The meniscus cartilages act as shock absorbers and contouring structures within the knee joint. They are a softer cartilage than the hard articular cartilage (gristle) within the knee and are more prone to tearing. They have a poor blood supply, which affects their healing capacity.
Different patterns of tear can occur in the meniscus cartilages, producing different symptoms and signs, and requiring different treatment options. Very few tears are able to be sutured / repaired, with most requiring removal of the torn fragment (if surgery is required at all).
The amount of meniscus to be resected is dependent on the size of the tear, although as little is removed as possible to retain some of the shock-absorbing and joint-contouring function of the remaining meniscus
Patellofemoral Disease
Patients with softening or early arthritis of the back of the patella (kneecap) may obtain some improvement from knee arthroscopy. Patients with this condition may be advised by Dr Mackie to trial considerable periods of physiotherapy and quadriceps strengthening before contemplating the (occasionally used) option of arthroscopy. In later stages of arthritis arthroscopy may not be helpful.
If the cartilage on the surface of the patella or on the trochlea (the groove in the front of the femur, along which the patella runs) is rough – it may be shaved back to a smoother edge. This may reduce grinding sensations or pain in the back of the patella. It does however carry the disadvantage of thinning the cartilage slightly.
Chondral Pathology
The articular cartilage (hard cartilage surface on the femur and tibia) can be partially or fully eroded. This may be a result of a traumatic event or as a result of progressive early arthritis changes. In early stages (usually with only a small isolated area of damage) patients may be aware of catching type pain and swelling in the knee.
The cartilage edges may be smoothed back to provide a stable surface and to remove the loose fragments that may catch within the knee during movement. If cartilage damage is widespread within the knee (early arthritis) then debridement (cleaning of rough edges etc.) has been shown to have very little long-term benefit. In some patients a focus on non-operative management of arthritis (and ultimately a knee replacement) may be advised.
Photographs of the Knee
At the time of surgery photographs are taken of the inside of the knee and these are provided to patients at the time of discharge from hospital. A sheet demonstrating “normal” pictures and with a key to interpreting the photos is also provided. If photos are brought back to the postoperative appointment the findings will be better explained.
After Knee Arthroscopy
It will be necessary to rest for a while after coming around from the anaesthetic. The knee may feel stiff and sore and painkillers may be needed to relieve the discomfort. Crutches may be obtained if required although most patients limp for several days to 2 weeks but can fully-weight-bear through their knee without crutches.
If the operation has been planned as a day case, most people are able to go home once they have recovered from the anaesthetic. However, anyone who has a general anaesthetic will need to be driven home and have a responsible adult stay with them for the next 24 hours.
A general anaesthetic can temporarily affect co-ordination and reasoning skills, so people are advised to avoid driving, drinking alcohol, making any vital decisions or signing legal documents for 24 hours afterwards.
Before discharge, a nurse will give advice about caring for wounds and bathing. Physiotherapy is not generally required unless recovery is slow at the postoperative return to Dr. Mackie.
The joint is likely to be quite sore, so anyone who has this operation needs to be prepared to take it easy for at least a few days and avoid any strenuous exercise, lifting or carrying. Driving should be avoided for the first 24 - 48 hours. Once home, it may be necessary to continue taking painkillers. Medications are provided at discharge from hospital. Most patients are able to reduce painkiller use to simple Panadol within a few days.
There will be a dressing and an elasticated bandage over the operation sites, applying pressure to assist with healing. At the time of discharge from hospital most patients will be provided with a list of instructions on how to care for the knee over the first couple of weeks following surgery.
A postoperative review is usually planned at 1 – 2 weeks following surgery to review wounds, discuss the findings at surgery and to ensure no complications have occurred. Photographs taken at the time of surgery should be brought to the appointment.
There may be some discomfort from the joint, and some swelling, for around two weeks after surgery. This can last longer if the treatment has been for arthritis. Most people are able to return to work within a week after knee arthroscopy if in office duties although it may be longer if their job involves bending, lifting or carrying (e.g. Up to 4-6 weeks in heavy manual duties).
It's usually possible to go back to usual physical activities or sports after around 4 - 6 weeks. Dr. Mackie will provide more advice about this in each individual case.
Side Effects and Complications
Arthroscopy is a commonly performed and is generally a safe surgical procedure. For most people the benefits in terms of improved symptoms (or from having a clear diagnosis of a joint problem) are greater than the disadvantages. However, in order to give informed consent, anyone deciding whether or not to have this procedure needs to be aware of the possible side effects and the risk of complications.
Side effects are the unwanted but usually mild and temporary effects of an otherwise successful procedure. Examples of side effects include feeling sick as a result of the general anaesthetic, although medicines are available to help avoid this. For this operation, there is also likely to be some pain and stiffness around the joint, which may last a few weeks and can make moving around very uncomfortable to begin with. There will be small scars from the incisions.
Complications are unexpected problems that can occur during or after the operation. Most people are not affected, but the main possible complications of any surgery are excessive bleeding, infection or an unexpected reaction to the anaesthetic. Complications may require further treatment although fewer than 1 in every 100 knee arthroscopies are followed by any significant complication.
Infection
If patients experience increasing pain, swelling, redness, fevers or are generally unwell it is important to be reviewed early to ensure no infection has occurred. If an infection is suspected then most patients will be readmitted to hospital for antibiotics and may require a repeat operation to wash out the knee joint. Fewer than 1 in 500 patients will develop a significant infection after arthroscopy, however it can have a long treatment and recovery period. A significant knee infection can result in a knee with worse symptoms than prior to arthroscopy.
Numbness
A loss of feeling in the skin over the knee near the incisions can occur although is rarely troublesome. An area of skin smaller than the size of a 5 cent piece may remain numb.
Blood Clots
Uncommonly, a blood clot develops in the veins of one of the legs (deep vein thrombosis or DVT). To help prevent this, patients at a specific risk are given an injection of anti-coagulant (blood thinning) medication during the operation, and if risk is high they are advised to take aspirin daily for 2 weeks. If worsening pain in the calf is experienced during the first couple of weeks following surgery an ultrasound of the calf is required to look for a blood clot. If a large clot is identified, then patients will require a course (often 3 months) of a blood thinning medication.
Bleeding
Persistent bleeding from the small wounds can occasionally require repeat bandaging and local pressure although rarely persists beyond a few days. This occurs in fewer than 1 in 200 patients. Many patients will develop significant swelling within the knee as a result of internal bleeding which settles with time. If significant swelling persists beyond 2 weeks an anti-inflammatory medication should be used.
Internal Knee Damage
By observing continuously through the arthroscope most structures within the knee are well protected but rarely cartilage, nerve or vessel damage may occur.
Ongoing Pain
Despite arthroscopy intervention some patients will have persistent pain or other symptoms from their knee. Arthroscopy is not guaranteed to improve all patients but is generally offered to patients with a suspected pathology, which is highly likely to respond favorably to surgery.
In a very small number of patients it is possible that pain may be worsened, sometimes related to a condition called “Complex Regional Pain Syndrome”. Although rare after arthroscopy, this condition may require intensive physiotherapy and treatment by a pain-management specialist.
